It is a common misconception that heel spurs are the primary cause of heel pain. In reality, heel spurs, which are bony projections on the heel bone, are often found by having an X-ray taken, and cause pain in only 5 percent of individuals with them. The majority of heel pain is generally due to plantar fasciitis, an inflammation of the plantar fascia tissue which stretches from the heel to the toes. While many individuals with plantar fasciitis also have heel spurs, the pain is typically from the damaged plantar fascia, not the spurs themselves. Heel spur syndrome and plantar fasciitis share similar risk factors, like athletic stress, obesity, calf tightness, high arches, and possibly osteoarthritis. Both conditions often respond to non-surgical treatments, including rest, footwear changes, and stretching. If these do not work, injections or plantar fasciotomy surgery might be recommended, though the heel spur is typically not removed during surgery. If you have heel pain, it is strongly suggested that you make an appointment with a podiatrist for a proper diagnosis and correct treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Terri Quebedeaux, DPM from Agave Podiatry . Our doctor will do everything possible to treat your condition.
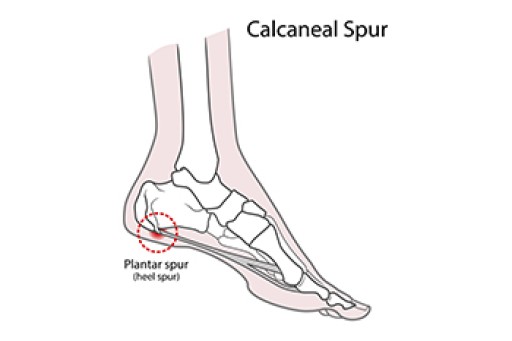
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Seguin, LaVernia, Gonzales, and Lockhart, TX . We offer the latest in diagnostic and treatment technology to meet your needs.